
Spring 2018
40 Years of SBM and the Biopsychosocial Model: With Middle Age Comes Thinking of the Next Generation of Population Health – From Microbes to the Masses
Karl J. Maier, PhD; Mustafa al’Absi, PhD; Reema Persad-Clem, PhD, MPH (cand)
It’s no coincidence that the 40th birthday of the Society of Behavioral Medicine (SBM) follows the 40-year anniversary of George Engle’s seminal 1977 paper introducing the biopsychosocial model. Some might argue that this work provided half of SBM’s DNA, so to speak.
As SBM reaches “middle age,” there are reasons to be pleased. SBM and the biopsychosocial model, born out of limits to Western medicine’s historic reductionism, have matured over 40 years through critical periods of development. The recent addition of psychosocial and behavioral content to the Medical College Admissions Test is one salient example.
Yet, the future is always unfolding. We are at a time of great innovation at the nano, molecular, and genetic levels, with discovery surrounding the human microbiome particularly exciting for its potential revolutionary significance to health. Surely, there are great hopes for all these advances. But ask any member of SBM, and there are limits to reducing health or disease to any one factor.
This contrast represents a bit of a “mid-life crisis” for us. How do we continue advocating for a holistic view of medicine in a time of unprecedented progress at the micro-level of intervention?
Well, crisis is opportunity. Bridging these historically competing narratives is not only possible, but necessary to fully address our most demanding health challenges. For example, today we find mounting evidence of epigenetic effects on genes relevant to disease that emanate from proximal physiological systems to the most distal environments. Likewise, social integration, policies, and the broadest cultural and economic factors have long been considerations in population health for their impacts on health behavior and physiology. And, microbiome research is quickly linking together all of these systems in ways that could transform our understanding of health and disease.
In essence, the evolving body of knowledge in the biopsychosocial tradition is maturing into an ecological paradigm for understanding individual and population health – one spanning microbes to the broadest ecosystems (Maier & al’ Absi, 2017).
A biopsychosocial ecological paradigm makes explicit what many in SBM have long appreciated - that biological, psychological, and social factors interact in a dynamic way. In our view, hierarchical levels with fluid boundaries can also be discerned within each of these domains; the immediate level includes molecular, genetic, and neural processes that support proximal, higher-order systems involving our physiology, emotion, and even social integration. Intermediate factors such as our built environments, behaviors, and societal practices bridge the proximal to the most distal factors like our natural environments, attitudes and other high-level psychological constructs, and broad cultural, economic, and political influences on health.
The ecological view can help address in a holistic way some of the greatest challenges in medicine today - from non-communicable diseases like diabetes, asthma, and cancer, to emerging infectious and zoonotic diseases, and antibiotic resistance. These problems all can (and need to) be addressed on multiple fronts, from the smallest levels of the microbiome and genetics, to the broadest environmental, behavioral, and social domains like education and policy – things that surely excite anyone in population or public health!
Beyond SBM, global entities such as the World Health Organization have identified planetary health, and in particular biodiversity loss at all levels, to be the most critical threat to human health. Likewise, the One Health approach emphasizes the interdependence of human, environmental, and animal health. Collectively, mainstream medicine is beginning to appreciate the importance of an ecological view, for example, as reflected in recent findings of the The Rockefeller Foundation–Lancet Commission on planetary health. Finally, the US Precision Medicine Initiative with its All of Us Research Program will examine genetic, lifestyle, and environmental factors at an unprecedented scale of measured variables and observations.
As we mature into “middle age” an ecological perspective clarifies opportunities to engage from a broad, integrative, systems view that also incorporates the tremendous advances occurring at the micro level today. This of course resonates with SBM’s interdisciplinary heritage. But the technological and statistical tools becoming available to access these systems, from genomics to epidemiology, also complement SBM’s strategic emphasis on digital health, and SBM’s forward view on the importance of leveraging large-scale data.
So, as Engel’s offspring, the biopsychosocial ecological paradigm doesn’t fall far from the proverbial tree. As SBM continues to mature with next-generation micro-level discoveries, an ecological view embraces this progress and welcomes the major shifts of the broader medical community that increasingly reflect SBM’s longstanding motto: “the whole is greater than the sum of its parts.”
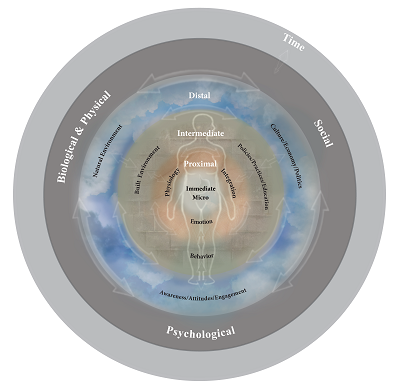
The biopsychosocial ecological framework extends Engel's (1977) original biopsychosocial concept by explicitly considering the dynamic relations across the biopsychosocial domains and their various levels, characterizing environmental and human factors as dynamic interactive processes that comprise a global ecological system over time. As an ecological system, the biological, psychological, and social factors are mutually determined and fluid between these domains and across levels of relative scale within each (immediate, proximal, intermediate, and distal). Population and individual health is thus a function of continual interactions among biopsychosocial domains and levels, from the most immediate micro-level factors to the broadest biological, psychological, and social systems. Concept and copyright by Karl J. Maier, PhD. Illustrated by Design Dedeaux.
Source: Toward a Biopsychosocial Ecology of the Human Microbiome, Brain-Gut Axis, and Health Psychosomatic Medicine79(8):947-957, October 2017.