How Can Primary Care Teams Address Insomnia in the Context of Persistent Pain?

Written By: Alexander Young, MA - Doctoral Student, Our Lady of the Lake University; Jennifer Funderburk, PhD - Clinical Research Psychologist, VA Center for Integrated Healthcare
What is insomnia?
Insomnia is a broad term for the inability to have restorative sleep and is one of many sleep disorders. Symptoms of insomnia come in many forms such as difficulty falling asleep, staying asleep or both.
There are two main types of insomnia:
- Short-term insomnia, which usually lasts a few days to a week
- Chronic insomnia, which can last weeks to months
Insomnia is caused by many factors, but some medical conditions can contribute to sleeplessness. One of these overlapping medical conditions is chronic or persistent pain. We often do not sleep well when we are in pain, and for those who are in constant pain, sleep can be a struggle.
When we do not get adequate sleep, mental health issues can occur such as:
- Loss of concentration
- Anxiety
- Depression
- A variety of other mental health concerns
There are many different ways of treating insomnia, but one of the most effective is a therapy called Cognitive Behavioral Therapy for Insomnia or CBT-I. This therapy has been shown to be effective with patients even in the presence of persistent pain. Sleep medication is often available through your PCP; however, behavioral therapy is a first line approach prior to the start of medication. Sleeping medication often has a variety of side effects and may not be appropriate for certain individuals.
Chronic Pain
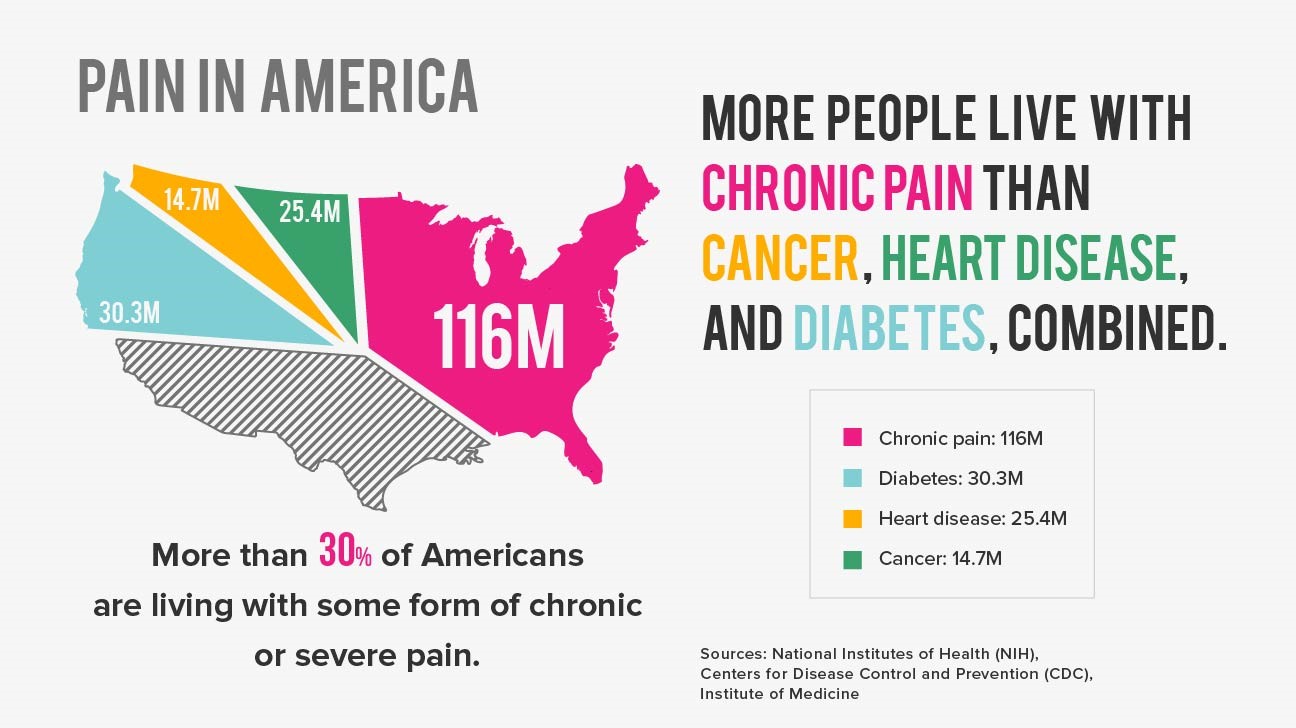
Chronic pain is a broad term that refers to several pain conditions that do not remit after a short period of time. More than 100 million Americans suffer from persistent pain and it is the leading cause of disability.
There is a high prevalence of sleep disorders in patients who have persistent pain. These two issues can cause a great deal of difficulty for patients seeking respite from their pain. It also creates a growing cycle of pain and sleeplessness which can manifest itself into greater mental health issues. Focusing on improving sleep can simultaneously improve patient’s ability to cope better with their pain.
Integrated Primary Care
Many people are unaware of the slow but steady integration of behavioral health services into primary care settings. This steady growth of an embedded service has shown to be an effective alternative to traditional mental health care. There are many models of this integration, but the most common is the Primary Care Behavioral Health (PCBH) model.
In this model, mental health professionals’ function as consultants, providing brief and targeted intervention to patients as directed by the PCP. There are many ways that a behavioral health professional in primary care might help someone suffering from insomnia while also dealing with persistent pain.
Insomnia Treatment
As mentioned previously, the primary treatment for insomnia is the use of CBT-I. Your provider can help design a treatment approach that will work for you and guide you through the necessary steps to get a better night's sleep.
Some simple interventions within CBT-I have shown to be helpful to patients dealing with insomnia and chronic pain.
Sleep Hygiene
This is a broad term that refers to actions we take before bed. These may include:
- Drinking water before bed
- Watching TV
- Drinking alcohol
- Staying on your cell phone
With sleep hygiene, your provider will work with you to reduce unhelpful actions and develop a plan to wind down prior to bed.
Relaxation Training
This refers to the large set of interventions that relax individuals prior to getting in bed. This could include:
- Meditation
- Mindfulness
- Progressive muscle relaxation.
This combined with sleep hygiene may make sleep more accessible and restorative. This intervention may also help with painful sensations that make it difficult to fall asleep.
Stimulus Control Therapy (Sleep Restriction)
This approach sets a strict sleep schedule using a specific set of rules to improve your sleep. An example of this would be always waking up at 7 a.m. regardless of your past nights’ sleep quality. This could also include eliminating naps or day sleeping and not getting into bed until you are sleepy.
Over time, this type of approach regulates the sleep cycle and encourages a better sleep schedule.
There are many natural insomnia treatments and approaches in CBT-I that can be helpful to those suffering from insomnia from chronic pain. By consulting with your Primary Care Physician (PCP), you can develop a plan that meets your specific needs prior to trying sleep medication.
More Articles

Insomnia in Older Adults: Tips to Master Sleep as We Age
How we sleep and how we can sleep better changes as we age. Check out these tips for older adults with poor sleep or insomnia.

Dangers of Sitting
Understand the dangers of sitting and how you can decrease the time spent sitting.


